August is psoriasis awareness month, so I thought I’d take some time to review a common question in the office. How can I treat my psoriasis?
Psoriasis is a very common disease. It affects about 2% of the US population. We treat patients with psoriasis every day. Most patients with psoriasis have red, pink areas of scaling skin. Psoriasis is a lifelong disorder. There is no cure. So, treatment is a continual process to keep it under control. Over the past twenty years, treatment options for psoriasis have greatly increased, making choosing a treatment more complex than ever. Let’s break it down. This is the mindset I use when trying to help a patient decide.
Where is your psoriasis? Psoriasis can be anywhere from the top of the head to the tip of the toes. Topical steroids are the traditional, initial and mainstay of psoriasis treatment. We use stronger ones in thick skin areas and milder ones in thin skin areas. There are additional newer topicals that are steroid free for areas where we are worried about the topical steroids weakening and thinning the skin.
Steroid free topicals include calcineurin inhibitors, tacrolimus ointment and pimecrolimus cream. These were originally designed to treat eczema but are widely used for lots of disorders in dermatology. Vitamin D topicals have been available for years as well, to use by themselves or in combination with steroids. Newer steroid free medications include Vtama and Zoryve. I have been particularly impressed with Zoryve for the eyelids. However, it is FDA covered only for thinner skin areas and is VERY expensive.
So, when choosing topicals we choose based on where it is located, how much of the body surface is involved, and what consistency would be best on that area of the skin. Topicals come in ointments, creams, gels, liquids and foams. For the scalp we will also sometimes recommend a medicated shampoo.
Are you sick and tired of it? Not a technical medical question, but patients often come and say, “I’m tired of dealing with this, is there anything else we can do?”. Frustration occurs for a few reasons, it is a chronic lifelong disorder which just is tiring over time. Inability or unfeasibility of treating large areas and disliking the consistency and feel of topicals on the skin are other reasons. For some, psoriasis great affects their quality of life, leading them to want to “do more”. For those who want to add something else my next suggestion is often light treatments.
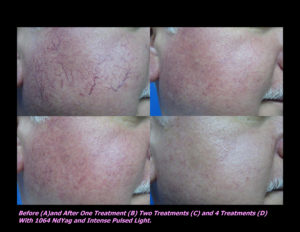
Psoriasis is usually well treated with UV light. In our office we have two stand up light booths and an Excimer XTRAC laser. All of these devices use the same type of UV light called Narrow Band UVB (NBUVB). NBUVB has been safely and successfully used to treat PS for over 20 years. Before that, and yes I’ve been around long enough to remember, we used Broad Band UVB and UVA.
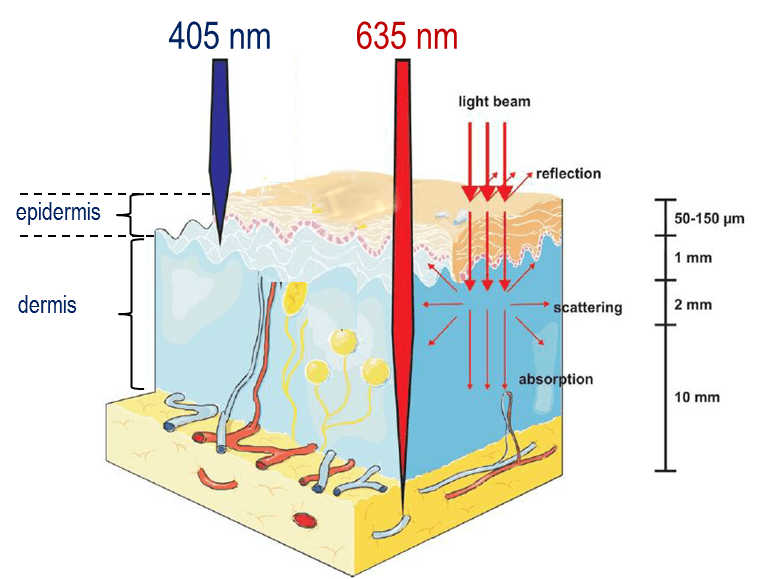
First, a quick review. Light is described technically by its wavelength in nanometers (nm). Outside light combines UVA (315-400nm) and UVB (280-315). NBUVB is 311-312nm. It is the wavelength of light that has been shown to be the most effective for most skin disorders. Tanning beds generally use UVA which is much less effective for psoriasis than NBUVB. But, in a pinch and during the summer outdoor sun will definitely help. It doesn’t take much, as little as 5-20 minutes 2-3 times per week outdoors.
In the office, we offer UV light treatments twice a week. Depending on the size of the area involved, some patients choose the light booth, and some choose XTRAC laser. Both laser and light booth are often covered by insurance. If paying out of pocket, laser is the more expensive of the two because it requires a technician and use of the XTRAC laser. In office treatments are quick, usually requiring less than 15 minutes of time in the office. Most patients see significant improvement in 20 treatments or less. After clearing we let each patient determine their need for maintenance depending on how long the skin stays clear. Some patients do maintenance once a week, some disappear for months and years and reappear once their skin starts flaring. We have had a light booth in the office since 2005. I have had the joy of seeing many patients have a life changing transformation from use of light to treat their psoriasis.
Limitations and risk of light treatments are collateral damage done to the surrounding skin by the UV light which can age and discolor the skin. Also, any UV exposure does add to our lifetime UV exposure which increases risk for skin cancer. However, it is very rare to develop skin cancer exclusively from controlled light treatments for psoriasis.
Do you have joint pain or arthritis? About 20-30% of patients with psoriasis also have psoriatic arthritis, a type of destructive arthritis. For these patients, topicals and light will not protect their joints. When using a medication that affects the whole body, we call that a “systemic” medication. That is where the myriad of treatment options get much more confusing for patients. So, we’ll dedicate a whole other article to Systemic Medications.
Finally, there are a ton of sites online that hope to sell you something to treat your psoriasis. The most unbiased and safe location online to learn about psoriasis and treatment options is the National Psoriasis Foundation website, www.psoriasis.org. I encourage you to check it out for information much more technical and detail beyond what is available here.















 Laser Vein Reduction Treatments
Laser Vein Reduction Treatments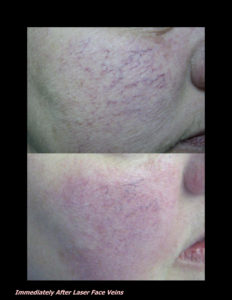












 DP Dermaceutical Products
DP Dermaceutical Products