Alopecia Areata (AA) is a type of hair loss that affects about 2% of the population. Most often patients have smooth round patches of hair loss. However, in more advanced cases, patients can lose all the hair on their body. Recent FDA approval of a new drug to treat AA encouraged me to write this update.
Alopecia areata results from inflammation around the root of the hair follicle. Inflammation prevents growth of hair and causes hair to fall out leaving smooth patches of hair loss
The exact cause of alopecia areata is not clear, but scientific advances have delineated that hair follicles are being attacked by a group of cells called CD8 T cells. The attack is triggered by an inflammatory pathway known as the JAK-STAT pathway. This discovery has led to the development of new drugs called JAK inhibitors that work to try to prevent the inflammation involved in alopecia areata as well as a number of other inflammatory conditions.
Although many things can trigger an episode of alopecia areata, those who are prone to alopecia areata will often experience a flare following times of high stress or illness.
Many scientists consider alopecia areata to be an autoimmune disorder, because it is the patient’s own immune cells that are attacking the hairs. A small percentage of patients with AA have other coexistent autoimmune disorders, such as autoimmune thyroid disease. Most patients do not have any other autoimmune disorders.
Treatment of alopecia areata is an area of continued research. Recently, a new drug was the first to be FDA approved specifically to treat Alopecia Areata. Many old and new treatments are still available and effective. We will highlight the most common treatments used in our office and those with a promising future.
Topical and Injectable Steroids– In the office, we often treat new onset alopecia areata with injection of a dilute steroid solution directly into the spot at one-month intervals. This stops the inflammation and allows the hairs to begin growing again. The actual amount of steroid injected is small and generally does not have any systemic effect on the rest of the body. A few injections may be required for complete regrowth. Topical steroids are sometimes used for follow up or at home treatment. Oral steroids are only used in diffuse and severe cases. For localized areas there is no therapeutic benefit of oral steroids over injectable steroids. Topical and injectable steroids work very well for over 95% of patients.
Sensitizing topicals – There are a number of topical agents that are applied to the area of alopecia areata with the intention of severe irritation. This severe irritation is designed to distract the immune system from continuing to attack the hairs. Dr Rosenberger does not tend to recommend this. For patients already stressing with hair loss, it is quite a difficult process.
Other Topical treatments – Other topicals are used to potentiate the effect of topical steroids. RetinA can be used to improve penetration and minoxidil (Rogaine) to increase anagen active growth of new hair.
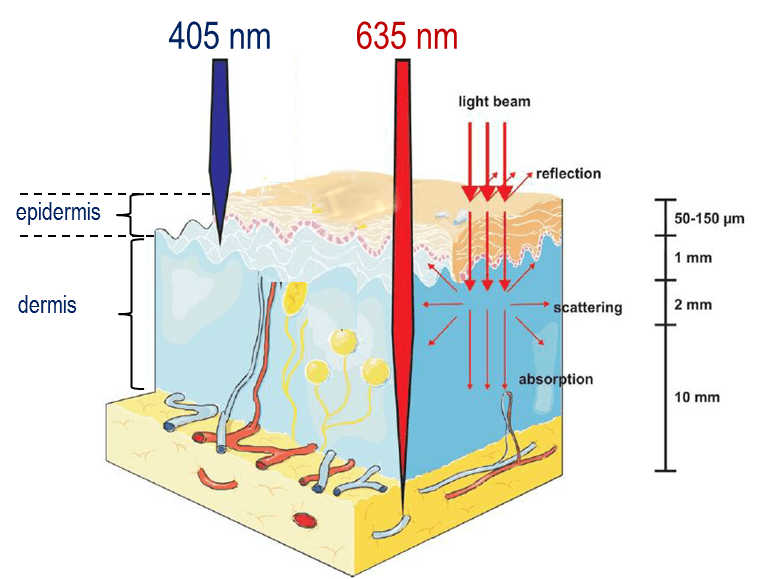
NEW – Excimer Laser treatments – Excimer Laser treatment uses NBUVB wavelengths of light directly targeted with a laser handpiece to the area. This is a good choice for children because it is painless. However, it requires twice weekly treatments until clear. Insurance coverage varies. We also use excimer laser to treat vitiligo and psoriasis in the office.
NEWER – Microneedling with Platelet Rich Plasma (PRP) or Topical steroids – Microneedling is a procedure that uses a device to puncture thousands of whole in the skin. There are a number of reports that show improvement of alopecia areata followed by PRP or topical steroids. However, these procedures are not well standardized and generally not much more effective than intralesional steroids. Cost is significant and out of pocket for most patients. Dr Rosenberger does offer microneedling for other conditions, but does not recommend it for AA.
NEWEST – JAK inhibitors- As mentioned above, JAK inhibitors block the JAK/STAT inflammatory pathway. This class of medicines is available in both topical creams and oral medications. When researching for this post, I found a study that showed that patients with AA respond 4-7 times better with oral JAK inhibitors compared to topical.
The JAK inhibitor approved for AA is oral Baricitinib (Olumiant), approved as a once daily pill for adults with severe AA. While patients did have good response, over 70% had at least a 50% improvement, the new drug has some issues. First, it is something that needs to be continued indefinitely. Over 75% of patients had recurrence of their AA within 12 weeks of stopping JAK inhibitors. Second, it is very expensive, with an estimated cost of over $50,000 per year. Last, there are side effects. The JAK/STAT pathway is important in a number of areas of the body, so inhibiting it has some significant possible side effects that include: increased risk of infection, increased risk of cancer and lymphoma, especially for anyone who has ever smoked, increased risk of blood clots, and increased risk of death for those 50 years and older.
Conclusion: Dr Rosenberger will continue to offer the standard treatment first line for patients with AA. JAK inhibitors should be reserved for those with severe AA, unresponsive to traditional treatment, and those willing to assume the risks stated in the drug’s label warnings.
Upon researching for this article though other thing really struck me. Multiple studies now have showed the strong association of AA with psychological disorders. One study showed that 78% of patients with AA have a psychologic disorder of some kind. Fifty percent of patients with AA have major depressive disorder and 39% have general anxiety. I have often noted to my patients that those with a “type A” personality are more likely to suffer with AA, but the above statistics are more alarming. The unanswered question remains what is the “chicken and the egg”. Which comes first? Nonetheless, I plan to use these statistics to emphasize the need for addressing mental health with my patients in the future. Patients who suffer with alopecia areata may find helpful support and information by joining the National Alopecia Areata Foundation. (NAAF)
___________________________________________________
If you know someone who may find this article helpful, please share it with them! Follow us on social media this week, and subscribe to our growing YouTube channel! If you would like to receive these posts in your email inbox, Subscribe to our Site.















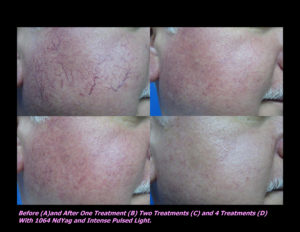
 Laser Vein Reduction Treatments
Laser Vein Reduction Treatments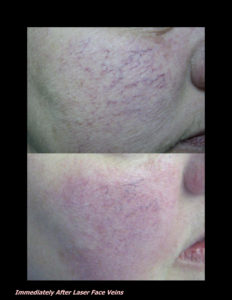












 DP Dermaceutical Products
DP Dermaceutical Products