August is Psoriasis Awareness Month, so I thought we would spend some time this week talking about the basics of psoriasis. These basic articles are what I like to call my “101” series. For collegiates starting an area of study, the first class you take when studying a particular subject, such as biology, is biology 101. So, here’s Psoriasis 101.
Psoriasis is a common disease that affects about 2% of the US population. We treat patients with psoriasis every day. Most patients with psoriasis have red, pink areas of scaling skin.
Psoriasis can be seen in larger areas of skin called plaques. Plaque psoriasis is usually seen on the elbows, knees, and scalp. In contrast, inverse psoriasis is usually smooth red areas of rash in the folds. Inverse psoriasis is often seen in the axillae, groin, inframammary area, abdominal folds, gluteal or buttock fold, and on the vulva. The other major type of psoriasis is called guttate psoriasis. Guttate means “resembling drops or raindrops.” These are often small red scaly plaques usually smaller than a nickel, spread all over the trunk and extremities, sometimes numbering in the hundreds.
In addition to these major types of psoriasis, sometimes psoriasis is described by the different areas of the body it impacts. Nail psoriasis and Scalp psoriasis are pretty self-explanatory. Palmoplantar pustular psoriasis affects the palms of the hands and the soles of the feet and often starts with pustules. Happily, psoriasis rarely affects the face. Sometimes eyelids are involved, but most other scaly rashes on the face are seborrheic dermatitis, aka dandruff, not psoriasis.
Psoriasis is not something that we cure, at least not yet. It is a disorder that some people are prone to having, just like having a center hair color or eye color. For those with a predisposition for psoriasis, the rash on the skin can be brought out by several triggers. Triggers include stress, illness of any kind, certain medications, and trauma to the skin. When psoriasis occurs at an area of prior trauma, we call this the Koebner phenomenon. The most common medicines to trigger a psoriasis outbreak are Beta-blockers, and the most common infection or illness to trigger psoriasis is a strep infection. A strep infection triggers a majority of cases of guttate psoriasis.
In addition to the rash on the skin, about 30% of patients with psoriasis have a destructive type of arthritis called psoriatic arthritis. The severity of arthritis is unrelated to the severity of the skin rash, and the joint pain is not necessarily on the same part of the body as the psoriasis rash. Patients with psoriatic arthritis need to be treated and followed by a rheumatologist due to the destructive nature of psoriatic arthritis. Although we often can control the rash with topical medications, systemic, oral, or injectable medications are often required to control arthritis and joint damage.
More recent data about psoriasis has shown that patients with psoriasis also have many comorbidities, which means that patients with psoriasis have a higher risk of diabetes, high blood pressure, and heart disease, to name a few. To learn more about comorbidities associated with psoriasis, see our previous article Comorbidities in Psoriasis.
Psoriasis treatment can vary based on how much of the skin is involved, where on the skin the psoriasis is located, the presence or absence of psoriatic arthritis, and MOST IMPORTANTLY, how much the rash is impacting a patient’s quality of life. What may not bother one person may cause severe social and emotional stress and anxiety for another. Another factor in treatment is the patient’s other medical problems, willingness to risk side effects, and preferences. Some patients despise creams; other patients hate shots. We try to provide treatment options that consider all these factors.
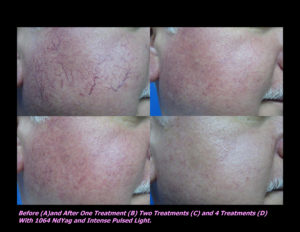
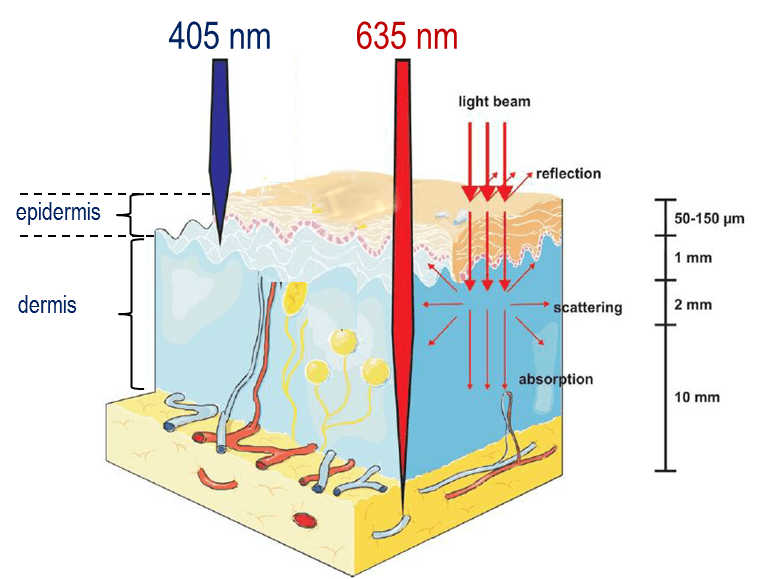
One doesn’t need to watch television for long to know that a myriad of treatment options exists for treating psoriasis. In short, the treatment options include topical medications, light and laser treatment, systemic medications, and newer biologic medications. The best NON-BIASED resource for reviewing treatment options and side effects is the National Psoriasis Foundation.
If you know someone who may find this article helpful, please share it with them! Follow us on social media this week, and subscribe to our growing YouTube channel! If you would like to receive these posts in your email inbox, Subscribe to our Site.















 Laser Vein Reduction Treatments
Laser Vein Reduction Treatments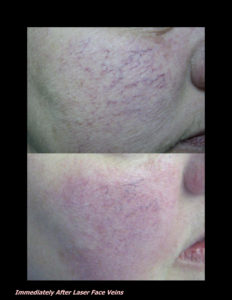












 DP Dermaceutical Products
DP Dermaceutical Products