What is a keloid?
A keloid is an overgrowth of scar tissue. An earlier stage of keloid is an overgrown, or hypertrophic scar. Following any injury of the skin, the skin’s natural repair process leads to healing of the wound. The healing process is designed to fill in the void that is created by the wound. As a simplification, in keloidal scarring, the scar tissue continues to grow even after the void is filled. This leads to an elevated overgrowth of scar tissue.
How can I tell if my scar is a keloid?
As compared to normal scars, keloids look and feel different. Keloids are often a raised, pink, smooth scar that can be tender or itchy. By definition, keloids overgrow out of the boundaries of the site of a normal scar. In times of severe overgrowth, scar tissue can limit movement and range of motion in areas like the neck, shoulders, and chest.
hypertrophic scar
Where do keloids most often occur?
Keloids most often occur on upper arms, chest, upper back, ears, and neck; they are less common on limbs, scalp, and face.
When do they grow?
Keloids often don’t start growing right away. They often take a few months to start growing after an injury. For this reason, Dr. Rosenberger likes to see patients back at three months following skin cancer removal to check for keloidal scarring.
early keloid in an excisional wound
Is there anything that can be done to avoid a keloid developing? i.e., procedural technique or wound care?
Generally, no. Keloids occur in some people independent of the technique used. For those prone to keloids, it is recommended to avoid all unnecessary wounds and procedures. Most doctors agree that proper wound care to expedite healing is the best advice. Some studies have shown that daily applying silicone sheeting to the wound after it has healed may reduce the incidence of keloidal scarring.
Can you remove a keloid?
Surgically removing keloids is usually not recommended because often the keloid grows back even larger post-surgery.
What treatments are available for keloids?
Topical steroids – If caught early, in the hypertrophic scar stage, a strong topical steroid can stop the development of a keloid. Dr. Rosenberger will often prescribe a topical steroid at the first sign of a scar misbehaving.
Intralesional Steroids – Once a scar is a true keloid, growing outside of the boundaries of the original scar, more intervention is usually needed. Small amounts of steroid are injected into the keloid to reduce and stop the growth of the scar tissue. Most early keloids regress with just a few treatments. More advanced keloids may require multiple treatments, usually administered at monthly intervals.
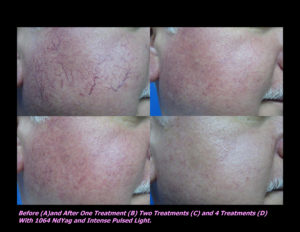
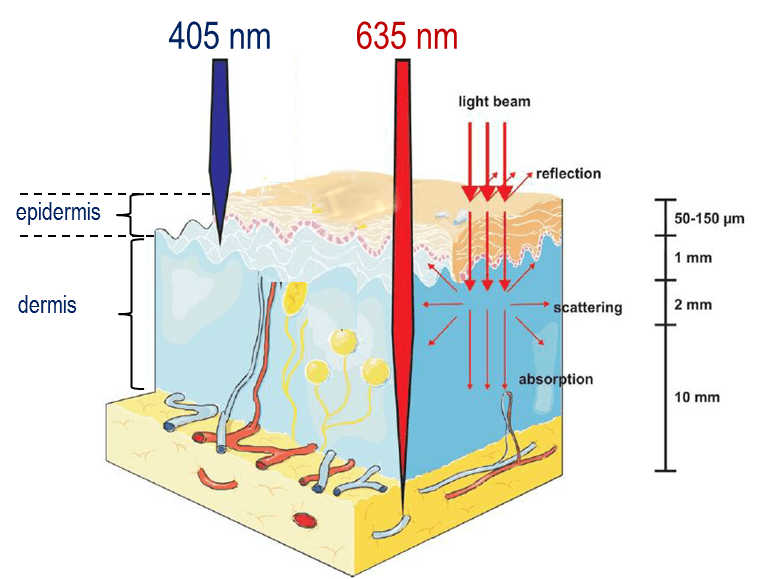
Pressure therapy – Pressure therapy involves adhering a silicone pad or other item over top of the keloid. Pressure on the keloid limits growth, but often won’t lead to a total resolution.Laser treatments – A few different kinds of lasers can be used to treat the keloid. The goal with lasers is to target and reduce the blood supply to the keloid.
_______________________________________________________________________
If you find these blog posts helpful, please share them on facebook, twitter or your social media preference using the buttons below. Also, you can email them to a friend.
Follow us on Facebook for event info, videos, and for the chance to win a FREE FACIAL!
If you would like to receive these posts in your email inbox, Subscribe to our Site!
















 Laser Vein Reduction Treatments
Laser Vein Reduction Treatments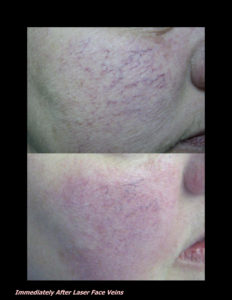












 DP Dermaceutical Products
DP Dermaceutical Products