August is psoriasis awareness month, so I thought I’d take some time to review a common question in the office. How can I treat my psoriasis?
Psoriasis is a very common disease. It affects about 2% of the US population. We treat patients with psoriasis every day. Most patients with psoriasis have red, pink areas of scaling skin. Psoriasis is a lifelong disorder. There is no cure. So, treatment is a continual process to keep it under control. Over the past twenty years, treatment options for psoriasis have greatly increased, making choosing a treatment more complex than ever. Let’s break it down. This is the mindset I use when trying to help a patient decide.
In our previous article (LINK TO NEW URL from above), we discussed topical and light treatments for psoriasis. In that article we addressed a few questions that can help steer treatment options for psoriasis.
Where is your psoriasis? Treatment choices can vary depending on what areas of the body are involved and how much of the body is involved.
Are you sick and tired of it? Treating psoriasis can get exhausting for people, and for many it can affect their quality of life. This can lead to a desire to “do more”.
Do you have joint pain or arthritis? About 20-30% of patients with psoriasis also have psoriatic arthritis, a destructive type of arthritis. It is important to recognize and treat psoriatic arthritis along with the help of a rheumatologist to find the best treatment option to both treat the skin and protect the joints. To treat the joints, we need to use “systemic medications” that affect the whole body usually by pill or by shot.
When I first started in dermatology, systemic treatment options were very limited. We had oral medications including Methotrexate, Soriatane, and Cyclosporin. Of these, only methotrexate also treated the joints. Methotrexate is a good, cheap, effective drug that is older than I am. However, it can irritate the liver and can rarely affect the lungs and blood counts. Because of that it requires strict monitoring, with visits and bloodwork every three months. I rarely use any of these medications anymore, because of these risks and the better options we have.
Are you willing to take a shot or do you want something oral? For many people with needle phobia, this question is a serious game changer. Many have zero desire to give themselves a shot. However, some of the newer drugs only require one injection every three months for maintenance and have high clearance rates that are tempting.
How much risk are you willing to take? Ask a risk adverse person, I understand the desire to assume as little risk as possible. This is why I often recommend exhausting topical options before proceeding to systemics for patients without psoriatic arthritis. Most of the newer medications are much less risky than the traditional option of methotrexate, but most do suppress the immune system somewhat. Almost all systemic medications for psoriasis include increased risk for lymphoma and mood changes because those things are more common in all patients with psoriasis.
Are you willing to have some immune suppression? Other than topicals, UV light and Otezla, all medications for psoriasis suppress the immune system somewhat. During the peak of COVID infections, this was often understandably a big issue for patients. For patients starting systemic medications, a blood or PPD test to determine prior exposure to tuberculosis is required. Depending on the patient’s history, some medications require checking for exposure to hepatitis as well. If a patient wants to avoid immune suppression, we stick to topicals, light and Otezla. If they are willing to assume some immune suppression risk, we consider the “biologics”
How stable is your GI tract? Any other major medical problems? Of the oral options, I often recommend Otezla as my first line choice. Major side effects include stomach upset and diarrhea leading to some weight loss. Other than that, mood change is the only other possible side effect. There is no blood test monitoring with Otezla and no suppression of the immune system, so that is why I often recommend it for those who can tolerate it. I usually initially provide my patients with samples to see if they are able to tolerate it. Other oral options, such as Rinvoq are in the class of JAK inhibitors, are not recommended for those with risk factors for heart disease, which eliminates a lot of us.
What is your insurance? All of these systemic medications other than methotrexate are EXPENSIVE. There are patient assistance programs and samples available. But most of them cost around $20,000 or more a year. While I never want insurance companies and financial matters to limit patients’ choices, there is some practicality that needs to be figured in. I start by prescribing the drug that seems to best fit the patient’s needs and desires FIRST. Then, sometimes we need to back track if insurance requires an additional drug to be tried.
Is there a particular drug you are interested in? I find many patients are interested in a certain drug they saw on TV or other ad. This is why drug manufacturers spent all those marketing dollars. Some patients know or have heard of a friend or acquaintance who was treated with a certain drug. If a patient is set on trying a particular drug and there are no contraindications to that drug, we consider it. If they ask my opinion, I usually share it. “If I had psoriasis that was affecting my quality of life and I had tried all of the lower risk options, I would want the drug that has been proven to have the highest clearance for the highest number of patients”. In most studies, patients have the highest clearance with what are called IL17 inhibitors.
While I am trying to not be too overly biased in this post, I’m sharing what I share with patients every day, and how I proceed through a process of how they can intelligently choose the option that best fits their needs and desires. If you or someone you know is struggling with their quality of life hopefully this outline of the decision making process will be helpful.
To learn more about all of the specific drugs, I recommend first visiting the National Psoriasis Foundation website for a non-biased reference at www.psoriasis.org.














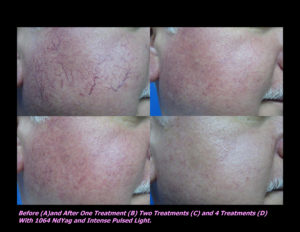
 Laser Vein Reduction Treatments
Laser Vein Reduction Treatments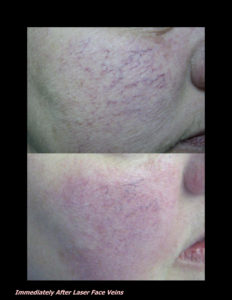












 DP Dermaceutical Products
DP Dermaceutical Products