There are two new types of genetic testing that utilize in the office for our patients. These tests should help aid in more accurate prediction of metastatic risk for early melanomas.
A little background in my simple terms… Along the base of the epidermis, the outer layer of the skin, we have cells called melanocytes that produce pigment in the skin. When these pigment cells multiply and grow in clumps they make a nevus, aka benign mole. When these same pigment cells multiply and grow cancerous they make a melanoma, a deadly form of cancer. The problem is that sometimes when the pathologist ( the doctor who evaluates the specimen under the microscope) evaluates the specimen it often looks abnormal but not abnormal enough to call it cancer. These abnormal moles are scientifically called dysplastic or atypical.
The prognosis of an abnormal, dysplastic mole can vary depending on the degree of abnormality. Generally, the pathologist grades the level of abnormality as mild, moderate, or severe. The degree of abnormality is graded based on the arrangement of the cells, the size of the cells, and the overall appearance of the cells and their nuclei. Mild is not so bad, and many people have hundreds that are mildly abnormal. Moderate is in between. Severe is looking closer to the features that we see in melanoma. This grading system is very subjective. The problem is with the severely dysplastic ones. We want to make sure those very abnormal ones are indeed benign. Unfortunately, a biopsy is a snapshot in time. We sometimes cannot say from standard methods, which of these severely dysplastic nevi would progress to become a melanoma and which would stay benign forever. Because the follow-up and treatment of dysplastic nevi can vary greatly depending on the degree of abnormality, accurate grading of these lesions is essential. Let me digress and say that nerdy dermatologists have spent thousands of hours and thousands of pages trying to sort this out clearly, but there is still a lot of disagreement about the malignant potential of abnormal or dysplastic lesions.
This is where our first genetic test comes into play… We send out all of our pathology specimens to a company called Dermpath Diagnostics. We utilize their services because they are highly trained experts that specialize in skin pathology. Their level of expertise greatly exceeds that which can be found in most hospitals or general laboratories at no additional cost to our patients. They have a team that works together on difficult cases, and they use the most current scientific techniques to provide the most accurate diagnosis possible. One test that they are utilizing on more difficult cases of dysplastic nevi is called MyPath by Myriad Diagnostics, purchased by Castle Bioscience the maker of the other test we are discussing in 2021. MyPath is a genetic test done on the skin biopsy specimen that is sent to the dermatopathology laboratory. In difficult cases, where the dermatopathologist is unsure if the lesion is likely to remain benign or become malignant, this additional test can give a more accurate diagnosis. The result provided by this test is an objective, not subjective, numerical score that classifies a specimen as “likely benign, likely malignant, or indeterminant” with a great amount of certainty compared to traditional methods of analysis. This is NOT a test that is done on every specimen, just those with more severe suspicious features. It is up to the dermatopathologist to decide when this test is necessary to provide a more accurate diagnosis. Those that are “likely benign” can be treated more conservatively, and those that are “indeterminant or likely malignant” are treated with more aggressive excision of the lesion and closer follow-up evaluation. Our pathologists are now using this additional test to help provide the most accurate diagnosis possible.
The second test is also done on the skin specimen that is sent to the lab, but the purpose is a little different. This test is for lesions that already have been definitively diagnosed as melanoma. Traditionally, the staging of melanoma is directly related to how deep the melanoma grows into the skin (Breslow’s depth).
When I tell someone that they have melanoma, there is only one question in everyone’s mind. “How long do I have to live?” quickly followed by “What do we have to do to help me live longer?”. Luckily, most melanomas we diagnose in the office are the earliest stage, Stage 0, which has a great prognosis of 95% 10-year survival rate.
The next genetic test is for Stage 1 and 2 melanomas. In these stages, there is no evidence that the melanoma has spread to the internal organs. This new test determines the likelihood that early (Stage 1 and 2) melanomas will progress to be metastatic and deadly. The goal is to monitor and treat more aggressively those with higher metastatic potential. Melanoma DecisionDx is a new test offered by Castle Biosciences. This test is done on the biopsied skin specimen.
In the past, we have used a test called Sentinel Node Biopsy where we test the lymph node to see if there is any melanoma in the lymph nodes. This was the best method of predicting which melanomas were more likely to become deadly. Those with lymph node involvement traditionally receive more aggressive follow up and treatment than those without lymph node involvement. However, 2 out of 3 patients who develop fast progressing deadly metastatic disease had normal lymph nodes at the time of diagnosis. So, it would seem there is some room for improvement in accurately predicting which patients will need more aggressive therapy.
Melanoma DecisionDx analyzes the genetic expression of 31 genes known to be involved in melanoma. This test provides a value which predicts disease free survival.
Class 1 -Low Risk provides a 3% likelihood that the melanoma will spread to the internal organs in 5 years. In more simple terms, these melanomas are very unlikely to impact a patient’s life span. These patients will receive traditional monitoring.
Class 2 – High Risk provides a 69% likelihood of having metastatic disease to the internal organs within 5 years. In more simple terms, these patients are more likely to have a shortened life span, which may be lengthened by more aggressive treatment and monitoring.
To learn more, you can watch the following video or download an informational handout about Melanoma DecisionDx.
Of course, the best course of action for melanoma is prevention and early detection. However, it is wonderful to now be able to utilize these new tests with hopes to improve long term outcome and survival. If you have had a melanoma recently and you would like more information about utilizing these tests, please schedule an appointment to discuss this in more detail. If you have a friend or relative who has been recently diagnosed with melanoma, please share this vital information with them.
—————————————————
If you know someone who may find this article helpful, please share it with them! Follow us on social media this week, and subscribe to our growing YouTube channel!
If you would like to receive these posts in your email inbox, Subscribe to our Site.















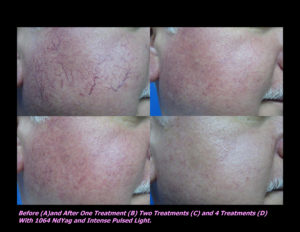
 Laser Vein Reduction Treatments
Laser Vein Reduction Treatments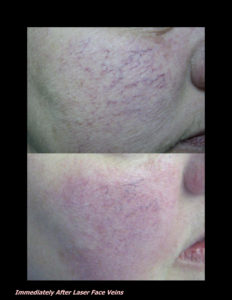











 DP Dermaceutical Products
DP Dermaceutical Products