Continuing with a theme of skin conditions that occur from skin to skin contact as we have discussed in our recent articles about swimming and wrestling, we will have a few posts about the viral infections of the skin.
There are three common types of viral infections in the skin. Herpes, warts, and molluscum are the ones we see almost every week in the dermatology office. We will discuss each of them in detail in upcoming posts.
Let’s start with herpes. While this may not be the most “pretty” topic, it is something with which most everyone can identify.
A widely quoted statistic from the NIH is that 90% of US adults have been affected by the herpes virus by age 50.
So, if you have been impacted by this virus. You are not alone. This article will answer the common questions I hear…
What is herpes?
Herpes is actually a group of viruses. There are actually eight different types of herpes viruses. The ones that most commonly affect the skin are HSV1 (oral herpes), HSV2 (genital herpes) and VZV (shingles and chickenpox).
How can I tell what kind of herpes it is?
Herpes simplex virus 1 (HSV1) is most often referred to as the oral herpes virus, causing what we traditionally call “cold sores” and HSV2 is most often referred to as the genital herpes virus. However, it is impossible to 100% differentiate the type of virus based on location or appearance. Patients often have herpes infections in less common places like feet, nose, fingers, ears and more. The only way to officially differentiate the virus type is a culture. However, generally, there is no medical need to distinguish the kind of virus, because the infection is treated the same independent of which of the three viruses above is causative. As we discussed in a previous article, shingles can also resemble herpes as well.
Is Herpes Contagious?
Herpes is contagious via skin to skin contact. If there is an opening or break in the skin, there is a higher risk of contracting the virus. Because it is so easy to contact and so prevalent, 90% of US adults have been affected by the virus in some way.
What is Asymptomatic Shedding?
Studies have shown that those infected with both HSV1 and HSV2 “shed” or spread viral particles in their saliva and genital secretions even when no active sore, lesion or rash is present. Shedding of the virus has been shown to be more common with HSV2 infections. Those who have had a previous HSV2 infection still shed and spread the virus as much as 50% of the time. Asymptomatic shedding can be greatly reduced by taking daily oral antiviral pills.
According to the Journal of Infectious Disease, “Although nothing short of abstinence can provide complete protection, the risk of transmission can be significantly reduced by both suppressive antiviral therapy and regular use of condoms.” Please share this information with your young loved ones!
Is there a vaccine for this virus?
No. There is a vaccine for other herpes viruses such as shingles and chicken pox, but there is not a vaccine for HSV1 and HSV2.
Once exposed to the virus, can I ever completely be cured?
No. The virus can reappear throughout one’s life.
What makes herpes lesions appear so suddenly?
After initial infection with the skin, the virus continues to live in the nerve that supplies that area of skin. The virus can be reactivated at times of stress or illness or by sunlight. Some patients even feel that certain foods trigger their cold sores to reappear.
How is herpes treated?
Herpes is treated with oral antiviral pills, acyclovir, famciclovir, and valacyclovir and topical antivirals. Often Dr. Rosenberger will recommend a loading dose of THREE Famciclovir 500mg at the first sign of herpes to shut down the reaction as quickly as possible. For those who are sexually active or kissing a partner that has not been exposed to HSV, daily antiviral pills can reduce the likelihood of infecting your partner. Dr. Rosenberger rarely prescribes or recommends topical antivirals because topicals are more expensive and less effective than oral treatment.
Are there any newer treatment options?
Yes. The newest treatment option for oral HSV is called Sitavig. Sitavig is applied inside the mouth near the area of the skin lesion. The pill attaches to the inside of the mouth and stays there ALL DAY until it dissolves, which can be 8-12 hours. The benefit of Sitavig is that it greatly reduces recurrences. On average, those who used one Sitavig pill were free of oral herpes for 304 days. The negative of Sitavig is that it is very expensive and insurances often don’t cover it. To learn more about Sitavig and how it works, check out their website.
Are there any supplements or dietary changes that can be helpful?
In general, it is believed that high arginine containing foods are more likely to trigger cold sores. In the lab, arginine increases growth of the herpes viruses and lysine inhibits arginine’s effect. Everything in moderation is always a good thought because arginine is a precursor to nitric oxide which plays a vital role in vascular health. Lysine works by blocking the effects of arginine. According to Harvard Women’s Health Watch, “ results of studies in humans have been inconclusive, and no standard dose has been determined. Research doses have ranged from 500 to 3,000 milligrams (mg) daily. Because scientific evidence isn’t solid, we can’t make a general recommendation about lysine supplements. Doses up to 3,000 mg per day aren’t likely to do any harm, but we have no long-term studies on these supplements. “
Although this may be considered a sensitive topic, as illustrated above, it is VERY COMMON in adults. As a parent or grandparent, consider sharing this information with your child or grandchild so we can reduce that statistic for our future generations.














 Laser Vein Reduction Treatments
Laser Vein Reduction Treatments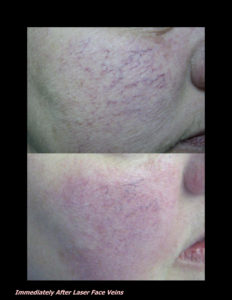












 DP Dermaceutical Products
DP Dermaceutical Products