The fancy name for hives
Urticaria is the fancy name for hives, which are a common problem in a dermatologist’s office. Usually, by the time patients come to me, they have had hives, itching, or some kind of rash for a long time. The milder cases of hives never end up in the dermatologist office.
What are hives? First of all, hives, by definition, come and go or at least move around in 24 hours. If you put a circle around a hive the next day, it should be gone out of that spot. The only exception is that sometimes there is residual irritation on the skin from scratching or what is used to attempt to treat the hives topically. They are usually VERY ITCHY and often unpredictable.
Can a biopsy tell you what is causing hives/urticaria? On a skin biopsy, urticaria will often show normal, just slightly swollen skin. A skin biopsy WILL NOT tell what caused the hives in the first place. If we biopsy a patient with urticaria, it is generally for one of two reasons. First, sometimes the patient has altered the skin so much with scratching and applying things topically, that it is hard to tell if it is just hives. Second, there is a more persistent variant of hives called urticarial vasculitis that also involves inflammation of the blood vessels.
What causes hives in the first place? Hives happen when something triggers cells in our skin called mast cells to release histamine. Histamine and a cascade of other mediators cause the localized swelling, redness, and itching in the skin known as hives. Hives can be triggered by all kinds of things heat, cold, light touch, pressure, vibration, and, of course, foods. There are also a few plants, such as stinging nettle, foods, and other chemicals that cause contact urticaria. However, 60% of all cases of chronic (>6 weeks) urticaria are idiopathic, meaning we never find a cause.
What is dermatographism? Dermatographism is a form of chronic hives often seen in patients with “sensitive skin”. Light touch or pressure can cause hives in streaks, handprints, and other unusual patterns.
How is anaphylaxis or angioedema related to hives? In angioedema and anaphylaxis, the hive-like reaction is much more severe, leading to the closing of the airway and even death. Patients with persistent urticaria are at higher risk of anaphylaxis and angioedema, so we recommend that they carry an EpiPen at all times. Technically, angioedema is affecting the deeper subcutaneous layers of the skin.
What lab tests are done for urticaria? For patients with new-onset chronic hives (>6 weeks), we often recommend checking a few labs. Dr. Rosenberger usually recommends checking the blood count, liver, kidneys, thyroid, vitamin D, and an ANA screening test for connective tissue disease. If you have hives, we recommend you see your regular doctor as well for a physical.
What are the treatments for urticaria? The mainstay of treatment for urticaria is avoiding know triggers and take antihistamines. For a more detailed discussion of antihistamines, see our most recent post. To try to suppress urticaria, Dr. Rosenberger often will recommend taking a long-acting antihistamine every single day for at least one month. If hives aren’t suppressed at standard doses, we sometimes increase the dose. If hives are suppressed, continue the antihistamine for at least a month. At some point, when the patient feels ready, Dr. Rosenberger will recommend stopping the antihistamine. If hives recur, resume the antihistamine. Patients often will need to take antihistamines for months before the issue resolves.
There are newer medications for patients for whom nothing else resolves their urticaria. A newer injectable called Xolair is available. For those with severe urticaria, carrying an EpiPen is recommended to treat angioedema or anaphylaxis should it occur.
If someone you know suffers from hives and you think this information is helpful, please share, and be sure to subscribe to our site!
|















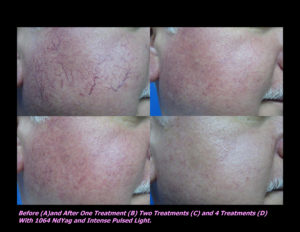
 Laser Vein Reduction Treatments
Laser Vein Reduction Treatments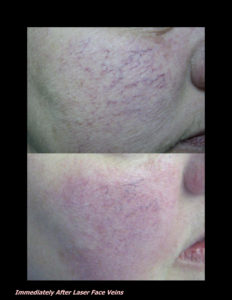











 DP Dermaceutical Products
DP Dermaceutical Products