Hyperhidrosis can be quite a problem for many patients. At its mild form, it’s a nuisance. At it’s most severe it can impair daily life functioning. In a previous article, we discussed types of hyperhidrosis and common causes.
In dermatology, we most often treat Primary Focal Hyperhidrosis. Primary, meaning there is no known underlying cause and focal, meaning that it occurs in a limited area. There are actual criteria for Primary Focal Hyperhidrosis. To learn more, see the article link below.
In treating Primary Focal Hyperhidrosis we are trying to reduce or inhibit production of sweat by eccrine glands in a limited area. In addition to regular or clinical strength antiperspirant, there are a few treatments that can help even more.
TOPICAL TREATMENTS
Topical treatments are applied to the skin to reduce sweat production. There is one major Rx medication to treat hyperhidrosis called Qbrexza. Qbrexza comes in a disposable cloth wipe and is applied to the skin once daily. It works as an anticholinergic, which means it can also cause dry mouth and dry eye if enough is absorbed systemically. While writing this article I learned more about a future option. Brella was FDA approved for underarm sweating in spring 2023, but is not yet commercially available. It is a patch that is applied for 3 minutes to the underarms in the doctor’s office. According to the International Hyperhidrosis Society, the Brella™ patch works via a method called targeted alkali thermolysis (TAT). TAT technology is based on the principle that heat is generated when sodium meets water. The result is that when the Brella™ sodium patch is applied to the underarm, there’s an interaction between the water in sweat and the sodium in the patch that generates a targeted amount of heat, causing microthermal injury to the sweat glands that inactivates those glands for a period of time. The process is non-invasive and does not involve needles. Results have been reported to last 2 to 4 months. As this is very new, we will be learning about cost and insurance coverage over the upcoming year.
Another “topical” treatment is called iontophoresis. Over many years Dr Rosenberger has had only a few patients achieve success with this because it requires purchasing a device and actually using it. Iontophoresis is primary for hands and feet. It involves using a device with a water bath and a mild current that decreases eccrine sweat production. This can be effective and has very low risk and side effects, but requires a significant time commitment of about 30 minutes 1-3 times per week. To learn more about iontophoresis, devices and tips and tricks, check out this LINK https://www.sweathelp.org/hyperhidrosis-treatments/iontophoresis.html.
In addition to these topical options there are a few more procedures that are more invasive.
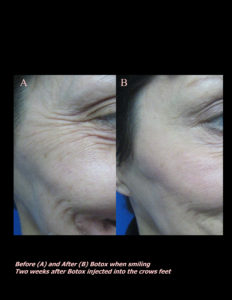
BOTOX injections for hyperhidrosis can be very effective, but not for those who are need shy or pain adverse. Over the past 15 years, Dr. Rosenberger has had a number of patients she has treated in the underarms, but very few in the hands and feet. The biggest risk in the hands is that some patients have muscle and grip weakness which can be detrimental to athletes or anyone who is serious about having a strong grip. Other than lots of needle sticks, BOTOX can also be quite expensive. Some insurances do cover the 750-1000 cost, but only after a labor intensive authorization and failure of all other methods. The benefit is that it works very, very well and dramatically reduces sweating for 3-9 months.
Miradry is a thermal device type treatment that is designed to permanently decrease sweating in the underarms. It requires a series of treatments priced at $2000-3000 and is generally not covered by insurances. This is not a procedure we offer at the office, but can be very effective. On there site, they report that the treatment can also decrease hair and apocrine (scent) gland production. To learn more check our www.miradry.com.
There are a number of oral medications that can reduce sweating as well. However, these have more side effects and Dr Rosenberger generally does not prescribe these because of their effects on other parts of the body other than skin.
These treatments are for those who topical OTC antiperspirants have been ineffective. To learn more about topical OTC options, check out our future article.
If you know someone who may find this article helpful, please share it with them! Follow us on social media this week, and subscribe to our growing YouTube channel! If you would like to receive these posts in your email inbox, Subscribe to our Site.















 Laser Vein Reduction Treatments
Laser Vein Reduction Treatments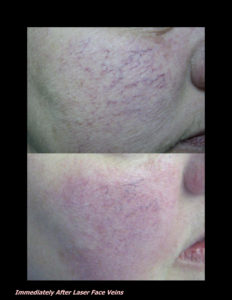












 DP Dermaceutical Products
DP Dermaceutical Products