Seborrheic Keratoses are the most common thing we see in the office each day. Here are the main questions we answer each day regarding this common growth.
Seborrheic Keratoses are the most common thing we see in the office each day. Here are the main questions we answer each day regarding this common growth.
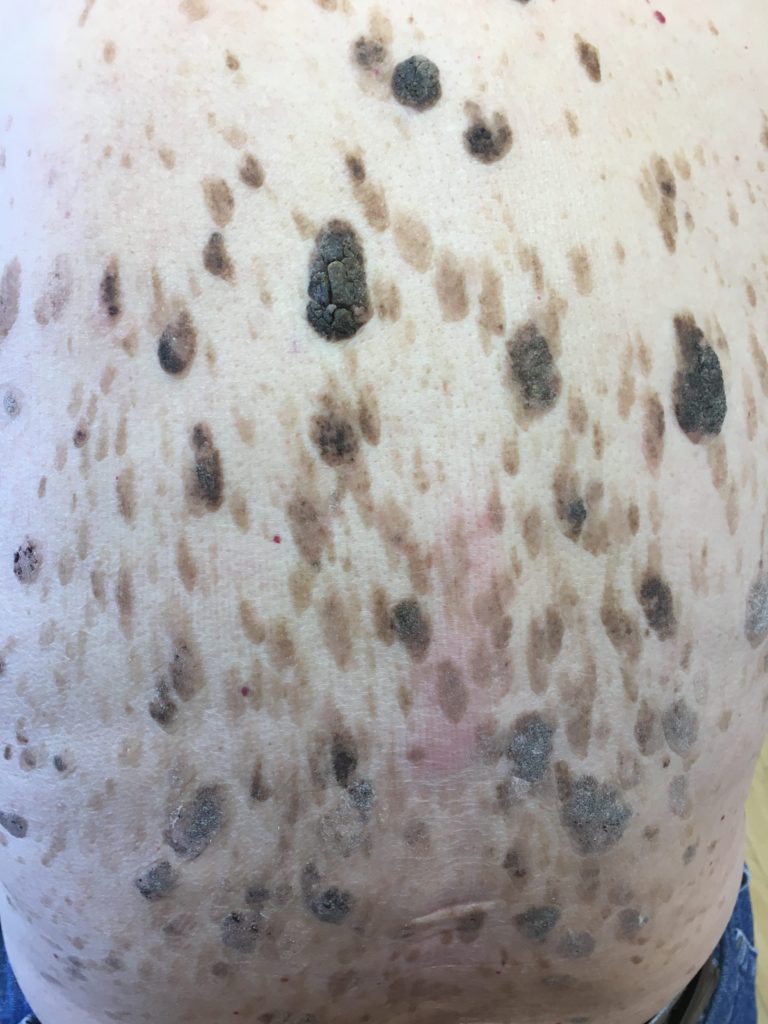
They are tan, brown, gray crusty growths that are most commonly seen on the back. They can be found everywhere on the skin except the palm and soles. Scalp, face, neck, under the bra line, back and legs are most common. They can be broad, over an inch in diameter, and they can be small and dangling. Two variants are Stucco Keratoses which are more white and appear on the legs and Dermatosis Papulosa Nigra that are dark brown appear on the cheeks of non-Caucasians. Most patients start growing Seborrheic Keratoses in their thirties and grow more and more with advancing age.
Are they cancerous? No, they are BENIGN. Because these lesions often meet the ABCDE criteria for melanoma, patients are often concerned about them. These lesions are often Asymmetric, have irregular Borders, change Color or have multiple Colors, are large in Diameter, and Evolve. So, why are they benign? Seborrheic Keratoses are a growth of the outer layer of the skin, versus true moles, and melanomas are a growth of the pigment cells of the skin.
Are they warts? The other concern patients often have is that these lesions are warts. Although they are often warty in texture, they are not true warts. True warts are caused by a virus called Human Papilloma Virus (HPV). Some Seborrheic Keratoses can get infected with the wart virus, but most have no associated virus.
Can we remove them? Yes and no. Yes, we can remove them, but in most cases, insurance will not cover removal. WHY? Seborrheic Keratoses are benign and of no harm to a person’s health. Exceptions include if the lesions look inflamed, suspicious, or are infected with the wart virus. This is a judgment call that the provider has to make. Everyone tells me their lesions itch and bother them. While I empathize, I cannot commit fraud. It is fraudulent to suggest to insurance companies that the lesions are medically necessary if they are not.
But I don’t like them, can I do anything about them? There is nothing a patient can do to prevent the development of the lesions. Not really.
But WE CAN! Lesions are most commonly treated with liquid nitrogen for cryosurgery or freezing. Frozen lesions get a blistery-like scab and take 7-21 days to fall off. Smaller lesions can be treated with Electrodessication or cautery for pinpoint accuracy.
The more the lesions are kept moist with Vaseline after treatment, the faster and better they heal and the less likely they will be to leave a noticeable scar. The most common negative of treatment is that it could leave some temporary or permanent discoloration.
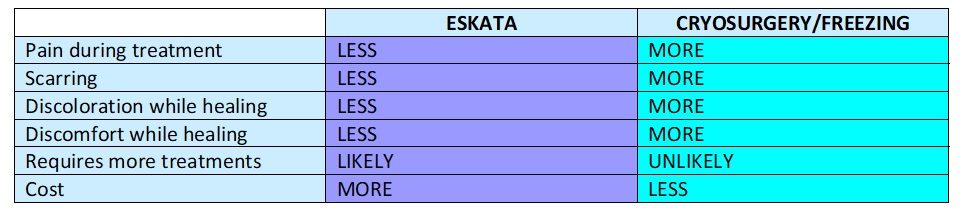
Is there anything new? YES, for the first time in my career there is something NEW! Eskata is a newly approved topical treatment that contains 40% hydrogen peroxide. It comes in a pen applicator and is applied to the lesions in a doctor’s office ONLY. Insurance companies will not cover the solution or the treatment with Eskata. Benefits claim to be less pain and less discoloration than with cryosurgery or electrodessication. The clinical trial showed 18% of patients had 3 out of 4 lesions completely clear. I personally am not too excited about that data, because it means patients will likely need multiple treatments. But, we will see how well it works in practice soon.
How much does treatment cost? We charge $15 each to treat the lesions in the office when using liquid nitrogen or electrodessication. When using Eskata, patients will need to purchase an Eskata applicator for treatment in addition to the $15 per lesion. Click here to learn more about Eskata, and schedule your appointment today!














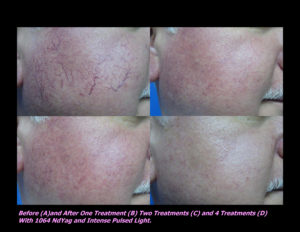
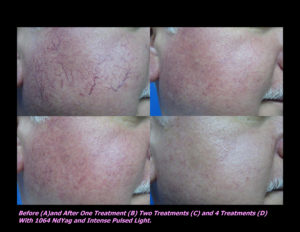
 Laser Vein Reduction Treatments
Laser Vein Reduction Treatments











 DP Dermaceutical Products
DP Dermaceutical Products