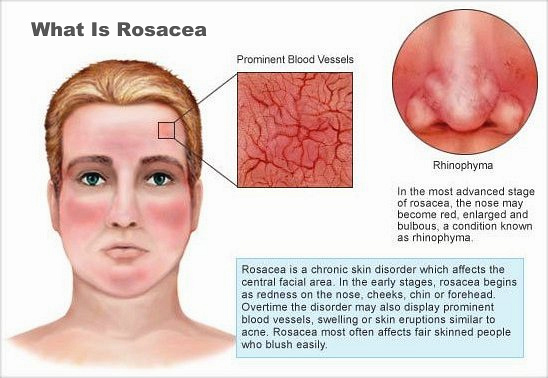
Rosacea has been reported to be associated with an increased incidence of a growing number of other disorders, including potentially life-threatening systemic illnesses such as coronary artery disease, high blood pressure, high cholesterol, diabetes, stroke, and even cancer. Wow!
Many studies have shown that people who have rosacea are statistically at a higher risk of having a number of other disorders and risks. We label these statistical findings as comorbidities. The official definition of comorbidity is “the simultaneous presence of two chronic diseases or conditions in a patient”. Why does this matter? This post evaluates the most recent comorbidity data for rosacea.
Considering that it is estimated that 16 million Americans have rosacea and 82% remain untreated, it may be of significance that we as dermatologists identify signs of rosacea even if that is not the patient’s presenting concern.
Here is my best current summary of the rosacea comorbidity data. I evaluated lots all of the current data. Listed below is the data that is the strongest. (2x means 2 times)
Cancer risk – In one study in Denmark, among the rosacea patients, there was no increased risk for malignant melanoma or ovarian, endometrial, cervical, esophageal, kidney, pancreatic or thyroid cancer compared to the general population. However, rosacea patients had a 42 percent increased risk of hepatic cancer, a 36 percent increased risk of non-melanoma skin cancer, and a 25 percent increased risk of breast cancer. Additionally, the study found rosacea patients were 22 percent less likely to be diagnosed with lung cancer than the general population. It is of importance to note that the risk of hepatic(liver) cancer is not related to alcohol use. Other studies also showed an increased risk of thyroid cancer and glioma.
Depression & Anxiety Disorder -2x increased risk (independent of alcohol use)
Migraine – 31% more likely
Inflammatory Bowel Disease (including Irritable bowel disorder, Crohn’s, Ulcerative Colitis, malabsorption & celiac) – 2x increased risk. A sensitivity analysis that examined the association between antibiotic treatment and subsequent IBD in patients with rosacea demonstrated that long-term frequent antibiotic users had a lower incidence of IBD, but without statistical significance.
Hypertension – 2-4x Increased risk of High Blood Pressure
Cardiovascular disease – 4x Increased risk, including Coronary Artery Disease and Heart Failure
Dyslipidemia –6x Increased risk
Diabetes – 2x Increased risk
Rheumatoid arthritis – 2x increased risk
Dementia & Parkinsons – two small studies showed an increased risk.
THANKS FOR THE GOOD NEWS! SO NOW WHAT?
The following recommendations were made in a recent article in the Journal of the American Academy of Dermatology.
Cardiovascular Disease – Monitor Blood Pressure, Consider family history of cardiovascular disease, Check fasting cholesterol and triglycerides and HbA1c at least once per year. Healthy diet and exercise.
Gastrointestinal Disease – Recommend evaluation by gastroenterologist if there are symptoms of bowel disease.
Psychological – Recommend evaluation by a counselor or psychiatrist if there are persistent symptoms of depression and anxiety.
Neurological – Recommend evaluation by a neurologist for signs and symptoms of dementia, Parkinson’s disease, migraine.
Malignancy – Yearly full skin examination, thyroid examination if symptomatic or enlargement or nodules are present. Keep up to date on age and sex appropriate malignancy scans (colonoscopy, prostate, breast, etc.)
Yearly blood work recommended – cholesterol, triglycerides, HbA1c, AST, ALT, GGT
Finally, the real question is… other than early detection, how can we reduce these comorbidities. One recent study addressed this question… “Effect of tetracyclines on the development of vascular disease in veterans with acne or rosacea: a retrospective cohort study”.
In this study, they looked at veterans with and without rosacea. Those with rosacea had increased vascular disease as compared to those with acne. For those with rosacea, there was a decreased incidence in vascular disease in those treated with tetracycline-class antibiotics (tetracycline, doxycycline, minocycline.) This is speculated to be related to the strong anti-inflammatory effect of this class of medications. Of the medications in this class, doxycycline has the strongest anti-inflammatory properties. Personally, this makes me very happy that I have taken low dose doxycycline for the past 15 years for my rosacea. Given the extremely low risk associated with taking low dose doxycycline daily, I think it is reasonable to continue taking it in attempts to reduce cardiovascular disease. I certainly will continue taking it myself.
Here is a link to one of the best online summaries of rosacea comorbidities that I found. The topic was also the subject of an intensive review in a recent Journal of the American Academy of Dermatology.
If you find these blog posts helpful, please share them on Facebook, Twitter or your social media preference using the buttons above. Also, you can email them to a friend.
If you would like to receive these posts in your email inbox Subscribe to our Site by clicking on this link.














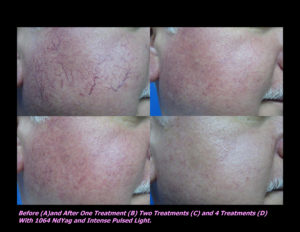
 Laser Vein Reduction Treatments
Laser Vein Reduction Treatments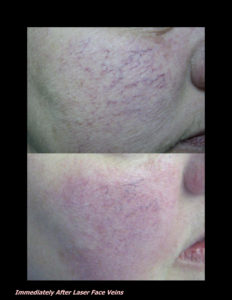












 DP Dermaceutical Products
DP Dermaceutical Products