If you’re living in WV like me, it’s finally cold outside. Now, to be honest, I despise the winter cold. I’m more of a spring girl myself. But I digress. Many of us were probably warned as kids so we didn’t get frostbite. But, what exactly is frostbite and its less serious dermatologic cousin, pernio?
Frostbite – True frostbite involves actually freezing of the skin. It is usually only seen after exposure to extreme temperatures and after prolonged exposure. It is most commonly seen in males and in those who might be unaware of the seriousness of the temperatures, such as the elderly, very young children, those with mental illness, or those with drug and alcohol addictions. There are three types of frostbite – first, second, and third-degree depending on the depth and extent of the freezing. Frostbite is most common in exposed areas such as the nose and ears and on the toes. Skin affected by frostbite is firm or hard to the touch and initially may look white or blue. Later stages involve blisters which predispose to secondary infection. Gangrene can occur as a final stage of more advanced frostbite, necessitating amputation of the involved area.
Frostbite treatment is best performed in a controlled setting and usually requires hospitalization. Proper slow rewarming in a warm water bath is the preferred initial treatment.
There are many other types of cold injury or response in the skin. The most common are cold urticaria (hives) and cold panniculitis. Cold panniculitis is seen on the lateral thigh of horseback riders and is used purposely in Coolsculpting to remove unwanted fat. Raynaud’s phenomenon is a spasming of blood vessels in the hands and feet in response to cold. Chilblains or Pernio is the more common cold-related skin problem seen in the dermatologist’s office.
Pernio – Also known as chilblains, pernio does not involve freezing of the skin. In contrast, pernio is usually seen in the spring and fall in cool temperatures and humid climates. I see it most commonly on those working out in their yard in the spring and fall. It is also more common in women and children who are more likely to be wearing sandals or flip-flops in shoulder seasons.
Pernio is a recurrent problem for some. It involves red, itchy tender bumps most often on the toes. The bumps usually progress to a small blister, followed by a dry hard crust weeks later. The initial stage usually lasts for 1-3 days and is best treated with a potent topical steroid. I generally recommend mupirocin antibiotic ointment in the later stages to prevent infection in the healing lesions.
There was a sharp increase in the number of cases of pernio seen early in the COVID-19 pandemic. This led to the term “COVID toes”. It involved the toes mostly of children who had little to no COVID-19 symptoms. Retrospective analysis of the cases of COVID toes showed that very few <15% actually tested positive for COVID-19. Two possibilities remain. COVID toes could be an extreme inflammatory response that develops after active infection with COVID-19. However, in retrospective analysis, many patients diagnosed with COVID toes both tested negative for the virus and for antibodies to the virus. The phenomenon more likely resulted from quarantining in spring with kids barefoot in their home and playing outside in the shoulder season more than normal. It will probably take many more years to know the real answer.
For all types of cold injury, avoidance and wearing warm, dry clothing and shoes is the primary goal. So, bundle up this winter!
—————–
If you know someone who may find this article helpful, please share it with them! Follow us on social media this week, and subscribe to our growing YouTube channel! If you would like to receive these posts in your email inbox, Subscribe to our Site.
















 Laser Vein Reduction Treatments
Laser Vein Reduction Treatments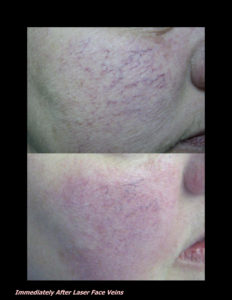











 DP Dermaceutical Products
DP Dermaceutical Products